My Last Day as Surgeon
Paul Kalanithi
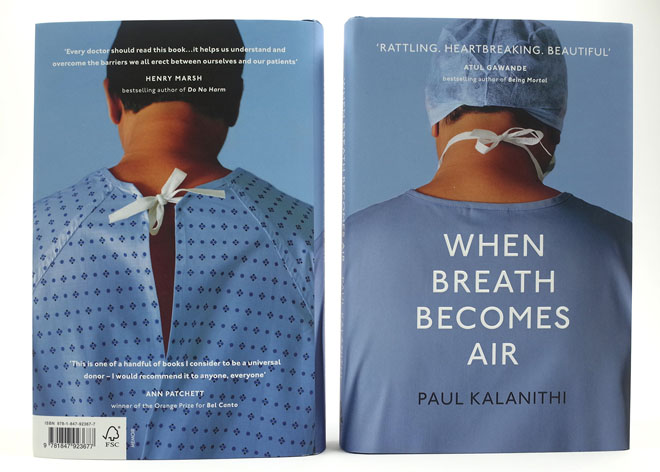
In the May of 2013, the Stanford University neurosurgical resident Paul Kalanithi was diagnosed with stage IV metastatic lung cancer. He was thirty –six year old. In his two remaining years- he died in March 2015- he continued with his medical training, became a father to a baby girl, and wrote beautifully about his experience facing mortality as a doctor and a patient. In this excerpt from his posthumously published memoir “When breath becomes Air” which is published by Random House, Kalanithi writes about his last day practicing medicine
I popped out of the CT scanner, seven months since I had returned to surgery. This would be my last scan before finishing residency, before becoming a father, before my future became real.
“Wanna take a look Doc?” the tech said. “Not right now” I said “ I’ve got a lot of work to do today. It was already 6 PM. I had to go see patients, organise tomorrow’s OR schedule, review films, dictate my clinic notes, check on my post ops, and so on. Around 8PM, I sat down in the neurosurgery office, next to a radiology viewing station, I turned it on, looked at my patients’ scans for the next day- two simple spine cases, finally typed in my own name. I zipped through the imagesas if they were a kid’s flip- book, comparing the new scan to the last. Everything looked the same, the old tumors remained exactly the same…except wait. I rolled back the images . Looked again. There it was. A new tumor, large,filling my right middle lobe. It looked oddly, like the full moon having almost cleared the horizon. Going back to the old images, I could make out the faintest trace of it, a ghostly harbinger now brought fully into the world.
I was neithe angry or scared. It simply was. It was the fact about the world, like the distance from the sun to the Earth. I drove home and told (my wife) Lucy. It was Thursday night and we couldn’t see (my oncologist) Emma again until Monday, but Lucy and I sat down in the living room, with our laptops, and mapped out the next steps: biopsies, tests, chemotherapy. The treatments this time would be tougher to endure, the possibility of a long life more remote. T.S Eliot once wrote “But at my back in a cold blast I hear/the rattle of bones, and chuckle spread from ear to ear” Neurosurgery would be impossible for a couple of weeks, perhaps months, perhaps forever. But we decided that all of that could wait to be real until Monday. Today was Thursday, and I’d already made tomorrow’s O.R. assignments; I planned on having one last day as a resident.
As I stepped out of my car at the hospital, at five-twenty the next morning, I inhaled deeply, smelling the eucalyptus and … was that pine? Hadn’t noticed that before. I met the resident team, assembled for morning rounds. We reviewed overnight events, new admissions, new scans, then went to see our patients before M. & M., or morbidity and mortality conference, a regular meeting in which the neurosurgeons gathered to review mistakes that had been made and cases that had gone wrong.
Afterward, I spent an extra couple of minutes with a patient, Mr. R. He had developed a rare syndrome, called Gerstmann’s, where, after I’d removed his brain tumor, he’d begun showing several specific deficits: an inability to write, to name fingers, to do arithmetic, to tell left from right. I’d seen it only once before, as a medical student, eight years ago, on one of the first patients I’d followed on the neurosurgical service. Like him, Mr. R. was euphoric—I wondered if that was part of the syndrome that no one had described before. Mr. R. was getting better, though: his speech had returned almost to normal, and his arithmetic was only slightly off. He’d likely make a full recovery.
The morning passed, and I scrubbed for my last case. Suddenly the moment felt enormous. My last time scrubbing? Perhaps this was it. I watched the suds drip off my arms, then down the drain. I entered the O.R., gowned up, and draped the patient, making sure the corners were sharp and neat. I wanted this case to be perfect. I opened the skin of his lower back. He was an elderly man whose spine had degenerated, compressing his nerve roots and causing severe pain. I pulled away the fat until the fascia appeared and I could feel the tips of his vertebrae. I opened the fascia and smoothly dissected the muscle away, until only the wide, glistening vertebrae showed up through the wound, clean and bloodless. The attending wandered in as I began to remove the lamina, the back wall of the vertebrae, whose bony overgrowths, along with ligaments beneath, were compressing the nerves.
“Looks good,” he said. “If you want to go to today’s conference, I can have the fellow come in and finish.” My back was beginning to ache. Why hadn’t I taken an extra dose of nsaids beforehand? This case should be quick, though. I was almost there. “Naw,” I said. “I want to finish the case.”The attending scrubbed in, and together we completed the bony removal. He began to pick away at the ligaments, beneath which lay the dura, which contained spinal fluid and the nerve roots. The most common error at this stage is tearing a hole in the dura. I worked on the opposite side. Out of the corner of my eye, I saw near his instrument a flash of blue—the dura starting to peek through. “Watch out!” I said, just as the mouth of his instrument bit into the dura. Clear spinal fluid began to fill the wound. I hadn’t had a leak in one of my cases in more than a year. Repairing it would take another hour. “Get the micro set out,” I said. “We have a leak.” By the time we finished the repair and removed the compressive soft tissue, my shoulders burned. The attending broke scrub, offered his apologies and said his thanks, and left me to close. The layers came together nicely. I began to suture the skin, using a running nylon stitch. Most surgeons used staples, but I was convinced that nylon had lower infection rates, and we would do this one, this final closure, my way. The skin came together perfectly, without tension, as if there had been no surgery at all. Good. One good thing.As we uncovered the patient, the scrub nurse, one with whom I hadn’t worked before, said, “You on call this weekend, Doc?”“Nope.” And possibly never again.
“Got any more cases today?” “Nope.” And possibly never again. “Shit, well, I guess that means this is a happy ending! Work’s done. I like happy endings, don’t you, Doc?”“Yeah. Yeah, I like happy endings.”I sat down by the computer to enter orders as the nurses cleaned and the anesthesiologists began to wake the patient. I had always jokingly threatened that when I was in charge, instead of the high-energy pop music everyone liked to play in the O.R., we’d listen exclusively to bossa nova. I put “Getz/Gilberto” on the radio, and the soft, sonorous sounds of a saxophone filled the room.
I left the O.R. shortly after, then gathered my things, which had accumulated over seven years of work—extra sets of clothes for the nights you don’t leave, toothbrushes, bars of soap, phone chargers, snacks, my skull model and collection of neurosurgery books, and so on. On second thought, I left my books behind. They’d be of more use here. On my way out to the parking lot, a fellow approached to ask me something, but his pager went off. He looked at it, waved, turned, and ran back in to the hospital—“I’ll catch you later!” he called over his shoulder. Tears welled up as I sat in the car, turned the key, and slowly pulled out into the street. I drove home, walked through the front door, hung up my white coat, and took off my I.D. badge. I pulled the battery out of my pager. I peeled off my scrubs and took a long shower.
Later that night, I called [my co-resident] Victoria and told her I wouldn’t be in on Monday, or possibly ever again, and wouldn’t be setting the O.R. schedule.“You know, I’ve been having this recurring nightmare that this day was coming,” she said. “I don’t know how you did this for so long.”
Paul Kalanithi is the author of the memoir “When Breath Becomes Air.”
Source: The New Yorker